TREATMENT OF SCHIZOPHRENIA
The term schizophrenia sounds like a severe endogenous-procedural mental
illness, which is accompanied by acute polymorphic psychotic episodes and an
increase in deficient symptoms and social and labor maladaptation between attacks.
To understand this complex crisis and very multifaceted disease, it is
necessary to understand a few concepts that sounded above. First, endogenous is
meant the presence in the human psyche and nervous system of some abnormal,
painful (pathological) process that leads to the development and progression of
the disease. This excludes a possible exogenous (external) cause (use of
surfactants, toxic, infectious lesions, etc.) of the psychotic state.
Procedural means, literally, the presence of the process of disease
development. In other words, schizophrenia is not an outbreak of inappropriate
behaviour that occurs suddenly and passes without a visible trace to the human
psyche. Instead, these are periodic polymorphic psychotic states that increase
deficient symptoms and maladaptation between attacks.
Deficiency symptoms, also known as "defects," are probably
the worst in this disease. The most pronounced, colourful, and violent
psychotic episodes are just episodes that are quite successfully stopped at the
present stage of the development of medicine (although it may take some time).
But each such episode or lack of maintenance treatment in remission leads to
increased apathy, lack of initiative, decreased willpower, emotional coldness,
and monotony. As a result, a person loses the desire and opportunity to go to
work, communicate with people, the range of interests and acquaintances over
the year’s narrows, and as a result, a person may become disabled
(schizophrenia - one of the diseases for which a disability group from III to
I, when a person is not able to take care of themselves).
The only way to survive would be regular care and supervision of
relatives or a typical stay in a psychiatric hospital. However, fortunately,
everything does not always end so sadly. With timely diagnosis, the beginning
of specific treatment, and the continuation of another as a supportive stage of
therapy, modern medicine allows you to successfully control the disease and
enable a person to return to a normal successful lifestyle. Then you can read
about the main symptoms and methods of treatment of this disease.
The main causes of schizophrenia
Unfortunately, the real causes of schizophrenia remain a mystery to
modern science. Schizophrenia is considered a multifactorial disease. In other
words, there are many known and unknown factors that can affect the occurrence
and course of the disease (environmental pollution, psychological trauma and
prolonged stress, hereditary predisposition, low social activity, use of
surfactants, etc.).
However, to identify among them one or at least a few basic is not
possible. The mechanism of symptoms is considered to be an imbalance in the
metabolism of the neurotransmitters dopamine and, to a lesser extent, serotonin
in the brain (and as a consequence, treatment is aimed at controlling these
processes), but this is only an explanation of symptoms, not the immediate
cause of the disease.
Schizophrenia is inherited - is it transmitted?
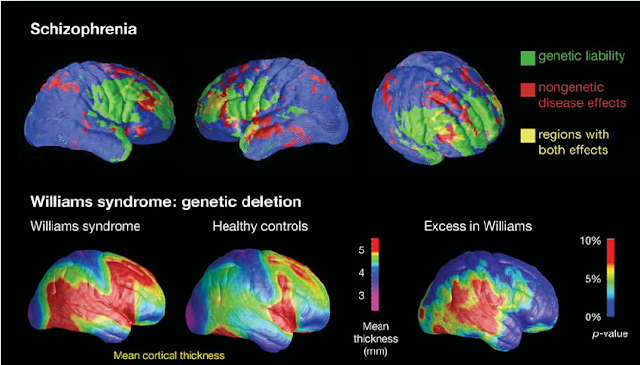
Recent studies show that people whose blood relatives have had a mental
illness (including schizophrenia) are statistically more likely to get it.
However, this probability is not 100%, but much less (data from different
studies differ). Moreover, it is believed that there is no "schizophrenia
gene," but there is a set of other genetic factors that can increase the
likelihood of the disease. Therefore, it is often impossible and impractical to
trace "where it all came from" because it does not affect the nature
of the treatment, and the transmission of such genes is possible for up to
seven generations.
The main thing that is important to understand is that the diagnosis of
"schizophrenia" is not a reason to abandon the prospect of having
children. On the other hand, even healthy parents can develop schizophrenia, as
the disease does not distinguish between well-being, status, and success.
Medical classification (types and types) of
schizophrenia
Schizophrenia is divided into several types depending on the predominant
symptoms and various kinds depending on the nature of the course. However, it
should be remembered that this division is quite conditional and often has no
significant impact on treatment selection. Therefore, in modern classifications
of mental illness, it is proposed to abandon the division of schizophrenia into
types, as it is not essential.
Before the general classification, it is necessary to allocate such
diagnoses as "schizotypal frustration" separately. It used to be
called "delayed schizophrenia." Still, then it was abandoned and
characterized by schizotypal disorder with a mild course, low susceptibility to
psychotic episodes, and often a positive prognosis due to a slight increase in
deficient symptoms.
Types of schizophrenia:
Paranoid
characterized by a predominance of "paranoid" or insane symptoms,
which may be accompanied by hallucinatory experiences in the form of well-known
in society "voices," as well as anxiety, agitation, insomnia,
inappropriate expressions, and behaviour.
Catatonic
characterized by the presence of motor retardation to the point of
stupor (a person can be for hours or days in a monotonous, seemingly
fantastically uncomfortable or bizarre position, not responding to speech,
refusing to eat), with a sudden spontaneous transition to meaningless,
unfocused possible aggressive behaviour.
Hebephrenic
characterized by a predominance of irrational, rude, inadequate,
almost childish behaviour. Often accompanied by sexual retardation. Relatively
poorly amenable to medical treatment.
Simple
probably the most insidious kind. Characterized by the absence of
psychotic episodes, the disease begins gradually and immediately with deficient
symptoms. Insidiousness is when the person and others notice the signs of the
disease when the process has gone far enough.
Types of flow
Continuous characterized by frequent psychotic episodes with virtually no
periods of remission, a rapid increase in deficient symptoms.
Episodic or recurrent is characterized by serial
psychotic states with long periods of remission and often no increase in
deficient symptoms.
Paroxysmal -progradient (fur coat (from the word fur coat - a blow in
German)) - occupies an intermediate position between the above types of flow.
The main symptoms and signs of schizophrenia
Most often, schizophrenia is characterized by a prodromal or incubation
period that can last from several weeks to several years and is not accompanied
by symptoms characteristic of schizophrenia. Still, during this period, you can
see some features. Next, we will consider these features in detail. Still, it
is worth remembering that the presence of one or even several such signs does
not indicate the presence of schizophrenia but is only a reason for
prophylactic purposes to consult a specialist.
The first signs of the disease may appear a few weeks or years (on
average 2-3 years) before the full onset of the disease. These signs
include:
- Valuable
ideas and hobbies - a person begins to pay much attention to mystical,
religious, and philosophical considerations, currents, up to
"fanaticism." This is also called metaphysical or philosophical
intoxication.
- Decrease
in ability to productive activity (work, training) - is shown in the form
of a reduction in motivation to action, a search of ephemeral sense in that
occurs, the general decrease in inactivity.
- Changes
in personality traits - a person's character traits can begin to change
for no apparent reason.
- Decreased
general activity, the need for communication, the desire for loneliness.
- Oddities
in behaviour.
The presence of one or more such signs does not mean the presence of the
disease, especially if such symptoms occur in adolescence, which is difficult
in all senses of the word, which significantly complicates the diagnosis of the
disease.
Directly the symptoms of schizophrenia are divided into positive
(productive) and negative (deficient). Consider them in more detail.
Disorders of thinking are singled out. Characteristic of the spectrum of
schizophrenic diseases manifested by a loss of purpose, the sequence of the
logic of mental activity. Such thinking disorders are called formal, as they
relate not to the content of thoughts but to the cognitive process itself.
First of all, it concerns the logical connection between ideas. In addition,
the imagery of thinking disappears, the tendency to abstraction and symbolism
prevails, there are breaks in thoughts, general impoverishment of thinking or
its unusualness with the originality of associations, up to meaningless. In the
later stages of the disease, the connection between thoughts is lost even
within a single phrase. This is manifested in the rupture of language, which
turns into a confusing set of passages of words that are completely unrelated.
There is an illogical transition from one thought to another ("slippage"),
which the patient himself does not notice. Disorders of thinking are also
expressed in the emergence of new bizarre words, understandable only to the
patient ("neologisms"), in fruitless reasoning on abstract topics, in
sophistication ("reasoning"), and in the disorder of the
generalization process, which is based on insignificant features. In addition,
there are violations such as an uncontrolled flow or two parallel streams of
thoughts.
It should be emphasized that formally the level of intelligence (IQ) in
people with schizophrenic spectrum differs only slightly from the IQ of healthy
people, i.e., intellectual functioning in this disease remains well preserved
for a long time, in contrast to specific impairments of cognitive functions
such as attention, ability to plan their actions, etc.
Less often, patients suffer from the possibility of solving problems and
problems that require new knowledge. Patients choose words according to their
formal features, without caring about the phrase's meaning, skip one question,
and answer another. Some thinking disorders appear only in the period of
exacerbation (psychosis) and disappear when the condition stabilizes. Others,
more stable, persist in remission, creating the so-called. Cognitive deficit.
Positive (productive) range of disorders: pathological
signs or symptoms acquired during the disease seem to be added to the patient's
mental state before the infection. These include:
Paranoid syndrome (paranoid) - characterized by the presence
of insane symptoms (delusional ideas). Delusional thoughts are conventionally
divided into several types: the idea of the relationship, persecution (known
in society as "mania of persecution"), poisoning, special
significance, influence, management. The content of these ideas can be very
individual and colourful. For example, some believe that he is being watched by
special services, distant relatives, and neighbours.
The very content of these ideas does not affect the nature of the
treatment. However, the range of these ideas can affect the danger to the
person and others. For example, if a person believes that his food is poisoned,
he may completely refuse to eat according to his painful inner logic. At the
same time, if a person believes that someone around him is doing these actions,
it may seem logical to clarify the relationship with the "offender,"
which can end in conflict, aggression, and many vague statements to the police.
Of course, a person does not always express such feelings aloud, but the presence
of such ideas can be assumed by delusional behaviour. For example, abrupt
refusal of food, communication with certain relatives, search in the housing of
the listening equipment, a search of imaginary pursuers (, a door eye),
protective actions (hanging of windows, barricading of doors). Brad can also be
hypochondriac (inadequate interpretation of sensations in the body, confidence
in the presence of serious and rare diseases, and combinations thereof).
Hallucinatory syndrome (hallucinations) - the presence of pseudo-hallucinations in humans (unlike real hallucinations, a person hears or feels hallucinations in his body and head). Most often represented by single or multiple voices of acquaintances and strangers in the head. Hallucinations can be periodic or permanent. The intensity or strength of hallucinations can also differ from barely audible and have little effect on the patient's condition to noisy. A person may fall into a hallucinatory stupor and not respond to external stimuli.
The content of these "voices," as delusional ideas, can be
very individual, but they are generally divided into several types. First,
commented - as the name implies, commenting on human actions and thoughts can
be positive (joke, praise) and sharply negative (scold, humiliate).
Advised - offer a person to perform certain actions, productive or unproductive.
Imperative - in contrast to the previous type of voice command to take
certain actions, resisting them is difficult, sometimes impossible. Acute
hallucinations can be both neutral and force a person to harm others and
themselves to commit suicide.
Hallucinatory symptoms are not always manifested by "voices,"
often in the form of bodily sensations, the feeling that external forces
control the human body or psyche.
A person's interpretation of hallucinatory experiences can also be
varied: some believe that the sensation results from exposure to
electromagnetic rays, the influence of intelligence equipment, the influence of
God or the Devil. The patient may also be accompanied by a sense of
"openness" of their thoughts to others and belief in the ability to
hear and influence the opinions of others.
As in the case of delusional ideas, people do not always express their
feelings aloud, but their presence can be assumed by unusual behaviour. For
example, the patient may not laugh, talk to himself or turn to an imaginary
interlocutor, listen to something, look around, close his ears and turn on the
music loudly to close off from these experiences.
Before negative (scarce) Circles are due to the painful
process of "loss" of the powerful layers of the psyche, which is
expressed in the change of character and personality traits due to the
weakening of the integrative activity of the central nervous system, patients
become lethargic, initiative, passive ("decrease in energy tone"),
they lose desire, motivation, desire, growing emotional deficit, appears
isolated from others, avoiding any social contacts. Sensitivity, sincerity,
delicacy is replaced in these cases by irritability, rudeness, uneasiness,
aggression. In addition, in more severe cases, patients have the disorders
mentioned above of thinking, which becomes unfocused, amorphous, meaningless.
Patients may lose so many former work skills that they have to register a
disability group.
Differences in the symptoms of schizophrenia in men
and women
There are no significant differences in the symptoms of schizophrenia in
men and women. Men are more prone to aggressive tendencies and actions, women
are prone to demonstrative behaviour, but given the high individuality in the
manifestations of the disease, these features are extremely relative. It is
believed that schizophrenia in women is more favourable, but it is not
significant compared to the timely diagnosis and provision of qualified medical
care.
Stages of schizophrenia
There is a prodromal (incubation stage) (from a few weeks to 2-3 years) when there are no obvious symptoms, but there are behavioural features described above. Most often ends with the emergence of psychosis or the so-called "debut" of the disease when the first appear meaningless and hallucinatory symptoms described above. The best doctors in USA provide more facilities in medical field.
Stage of "exacerbation" or psychotic states. It can begin
suddenly and violently within several days and in several weeks or months with
a gradual increase in symptoms. Very often, the first alarm signal is a sleep
disorder, although it is nonspecific. Psychotic states (psychosis) can last
from several days to several months depending on the individual, the severity
of the disease, and the presence or absence of medical care. Psychotic states
can be reduced (passed) without medical intervention (spontaneous biological
remission) but often turn into chronic psychosis, which is difficult to treat
and negatively affects the prognosis. At this stage, active treatment methods
are used.
Remission is the stage at which the symptoms of schizophrenia are absent or
minimal. If you follow the recommendations of experts and the presence of
supportive treatment, it is possible to return a person to his usual way of life,
social and labor activity. The quality and duration of remission depend
directly on exacerbation (psychotic state) treatment and support the treatment
phase. Maintenance therapy is not prescribed for several months in advance but
should be monitored depending on the patient's condition. There are two
important factors:
- Treatment
should be sufficient to maintain the person in a normal state;
- Treatment
should not interfere with a person's normal life and create excessive
discomfort.
Attacks of schizophrenia
An attack of schizophrenia ("exacerbation") is a psychotic
state (psychosis), which is accompanied by the appearance or intensification
(if in a state of remission to achieve a complete reduction of symptoms is not
possible) positive (productive) symptoms. The first psychotic episode in a
person's life is also called the onset of the disease.
Manifestations of psychosis are very individual, both between patients
and within one process. Psychosis can occur abruptly, literally over several
days, and gradually over several weeks and months. It is very important for the
patient to monitor his condition, as often, when others notice inadequacy in
behaviour, painful symptoms have been present for some time. The sooner a
person seeks help with symptoms of deterioration - the faster and more
effectively manage to cope with the situation. Most often, one of the first
alarming signs of damage is the deterioration of sleep, increased isolation,
anxiety. Subsequently, this is joined by meaningless and hallucinatory symptoms.
The greater the severity of symptoms, the less a person can control their
behaviour and the greater the likelihood that he will cross the conditional
"edge,"
In connection with the distortion of perception and mental processes, a
person can perform various inadequate and aggressive actions, because according
to his inner, painful logic (parallelisms), these actions are rational.
Sometimes patients under the influence of the disease can commit crimes, cause
property damage, themselves and others. A common mistake of relatives in such
situations is to convince the patient of his painful experiences. As mentioned
above, one of the characteristics of a ghost idea is the inability to
rationally or logically convince a person. Therefore, attempts to demonstrate
the falsity of experiences also fails.
For example, the patient claims that bandits who want to kill him hide
behind the front door. When demonstrating that there is no one at the door, a
person claims that the persecutors obscured around the corner. When no one is
around the corner, it turns out that they are already on the roof or waiting at
the front door, etc. Such attempts and the very fact of doubt in the reality of
the patient's experiences can cause irritation, anger, conflict. In contrast, it
is also impossible to "get involved" in painful experiences, confirm
them, encourage them, and take an active part. Given the unpredictability and
illogicality of inferences, relatives try to help so they can be involved in a
crazy structure. As a result, the patient may commit verbal and physical
aggression against them (demand and knock out confessions in conspiracy,
betrayal, etc.
Treatment of schizophrenia
Thanks to the development of medicine, significant progress has been
made in treating schizophrenia and mental disorders in general. The first drug
and the first neuroleptic for treatment appeared in the 50s of the twentieth
century, and it was chlorpromazine or Aminazine known in our region. For the
first time, this drug allowed psychiatry to restrict the patient's freedom in
anticipation of spontaneous improvement and affect the course of the disease
directly. This drug is morally and obsolete but still occupies its niche in
treating mental disorders and other emergencies. Another, perhaps much better-known
drug is Haloperidol. There are many horror stories and myths about this drug
(not all of them are unfounded), but it is still one of the most effective
drugs to treat acute psychotic states.
A huge number of neuroleptics of various properties and characteristics were synthesized. They all occupy a certain niche or, in other words, are the keys to opening the castle of mental disorder.
As a result of the high individuality of people not only in the personal and characterological but also in the biochemical sense, the task of the psychiatrist is a selection of "the same key." Complicating the job is the fact that neuroleptics have a range of specific side effects. However, side effects are not allergic reactions, and to predict the occurrence of side effects, it is impossible to do a skin allergy test (such as with antibiotics).
These side effects include neuroleptic or extrapyramidal syndrome,
akathisia, parkinsonism. They manifest in painful muscle spasms, such as the
inability to perform normal movements, tremors, anxiety, restlessness, and
restless physical sensations in the body and especially in the legs.
Inpatient treatment involves several important
components.
The first component: sedation. Involves the use of sedatives as
psychotic disorders may be accompanied by severe anxiety, agitation, insomnia.
As a result of their actions, a person can calm down, finally sleep, less
pronounced behavioural disorders. This component is very important and, in the
early stages, plays a leading role. The patient's relatives can often be
frightened by this stage as it is connected with the expressed drowsiness,
inhibition, passivity. However, this is necessary, and it is important to
remember that this phenomenon is temporary and will take place with the
abolition of drugs without harm to the psyche and the body as a whole.
Sometimes there is the opposite attitude: "it is enough for him / her to
sleep so that everything passes." This is not true. After waking up, the
symptoms flirt with renewed vigor. For this not to happen, the following
component is important.
The second component: the fight against productive symptoms. For this purpose,
neuroleptics of incisive action are used. They give a relatively little
soothing effect. Their task is to correct the biochemical imbalance, which is
the cause of delusions, hallucinations, emotional inadequacy. This effect is
not instantaneous, and neuroleptics take several days to work fully. It is not
uncommon for a person's condition to improve significantly after the first
dose, but it is no less rare for the desired result to have to wait several
days or even weeks. This component is associated with the highest probability
of side effects and must be under strict control. Drugs actively used in the
hospital do not always go to the maintenance treatment stage; very often, a
much softer and more comfortable drug is selected for a person.
The third component: tonic therapy and control of vital signs. Mental
illness sucks a huge amount of psychological and physical strength from the
body. The person is exhausted, cannot sleep properly, and regain strength,
appetite decreases. Therefore, it is necessary to fill the lack of vitamins,
nutrients, fluids.
The fourth component: involvement of related specialists. Being in a sick
state, a person tends to ignore cries for help from his body. As a result,
exacerbation of chronic somatic diseases, acquisition of new ones, including
injuries, is often observed. Fortunately, in the vast majority of cases, these
are not serious complications or life-threatening situations. However, if there
are problems and indications, the psychiatrist involves other specialists to
provide complete care.
The final stage of inpatient treatment is the selection of maintenance
therapy, which will promote the complete recovery of the person from the
disease, maintain it in the norm and prevent possible exacerbations. Unlike
many other areas of health in psychiatry, except for some conditions, it is not
possible to "go to the hospital drip" once or twice a year for
prevention. Maintenance therapy is a process that must be inseparable.
Otherwise, it can lead to significant deterioration. The nature of maintenance
therapy can be divided into two options: taking medication in tablet form and
taking depot drugs.




Comments
Post a Comment